An operating room lamp is a product most people can easily envision—its shape, purpose, and key attributes come to mind when thinking of a surgical light. Yet understanding what a surgical lamp truly is—or why operating lights have certain distinctive features—isn’t as straightforward.
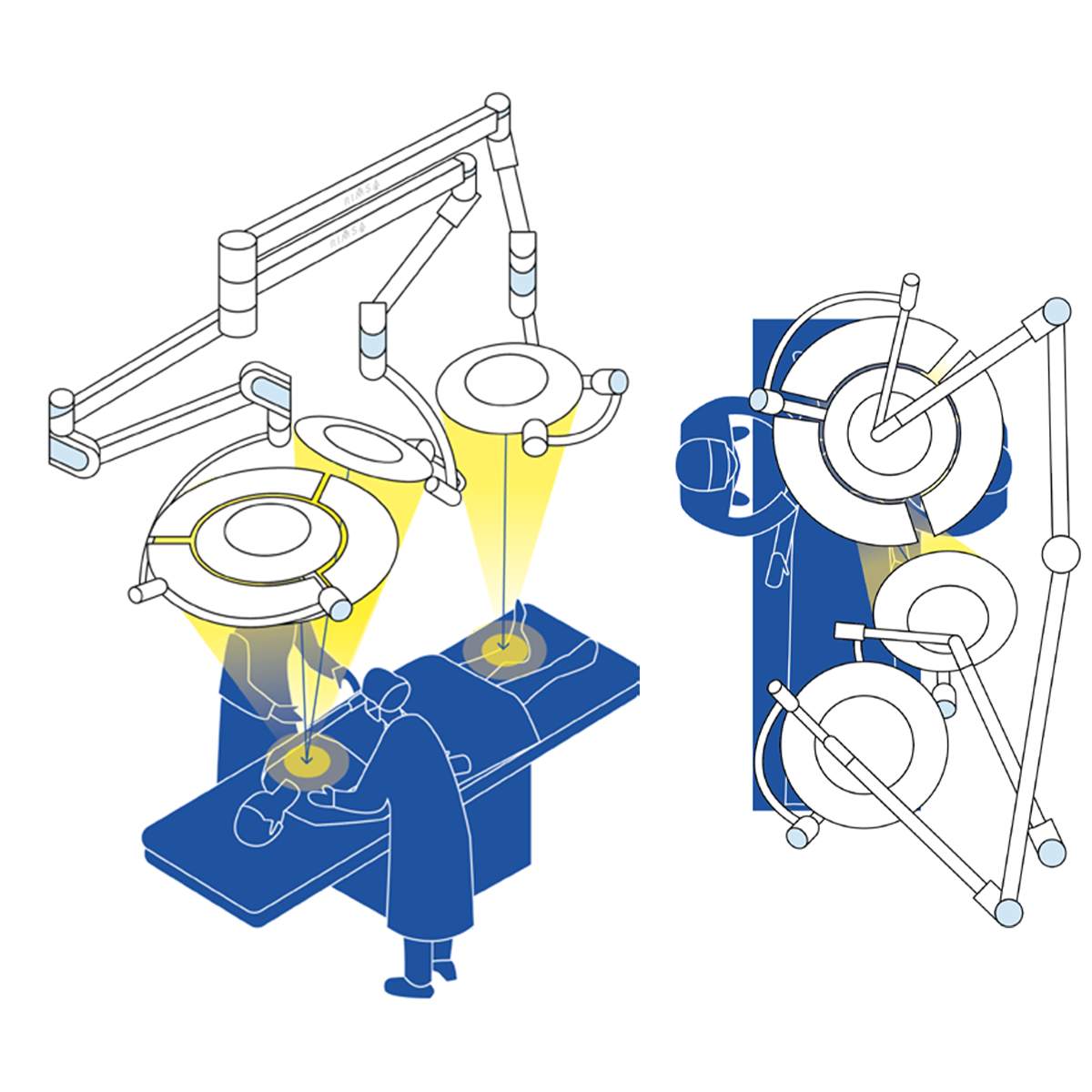
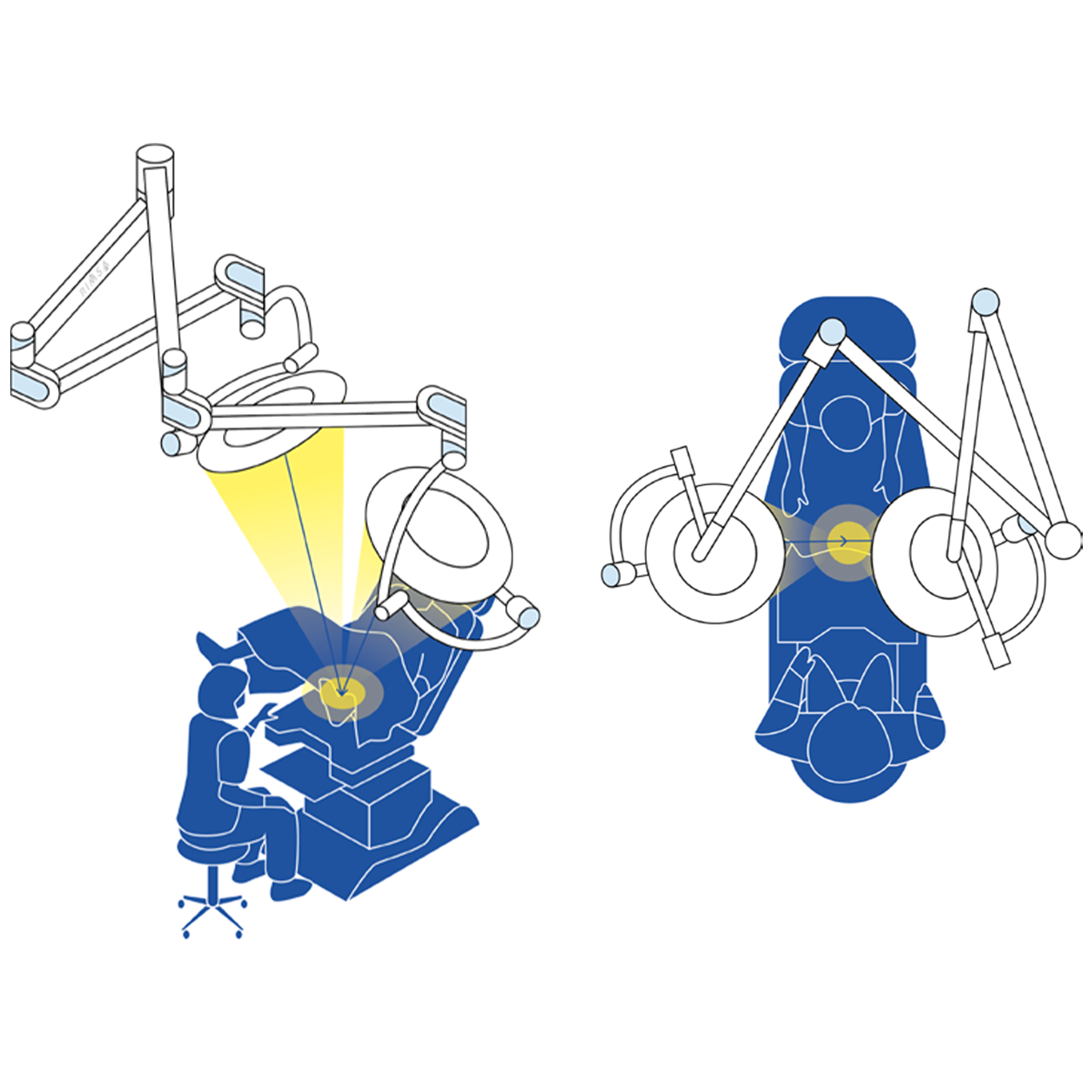
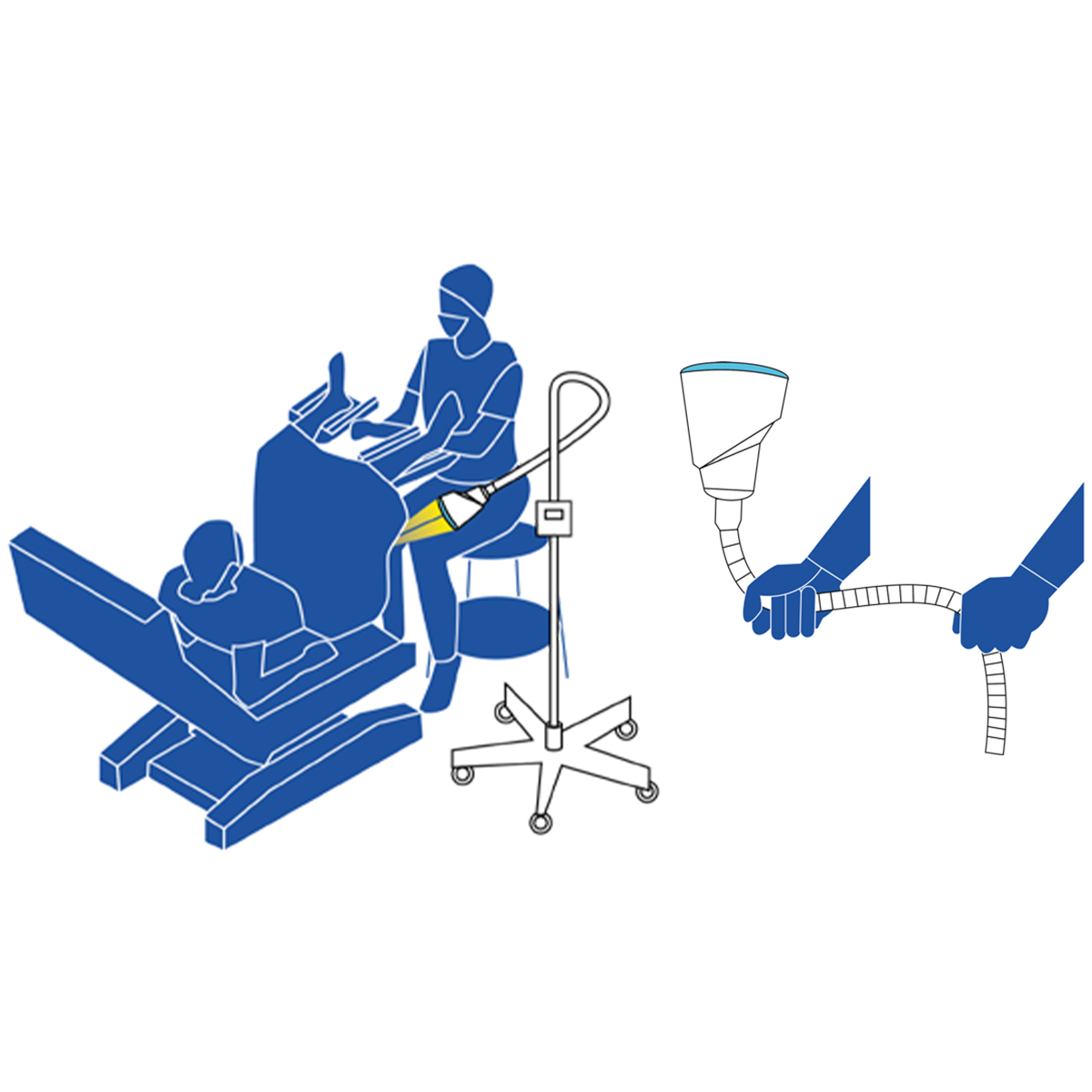
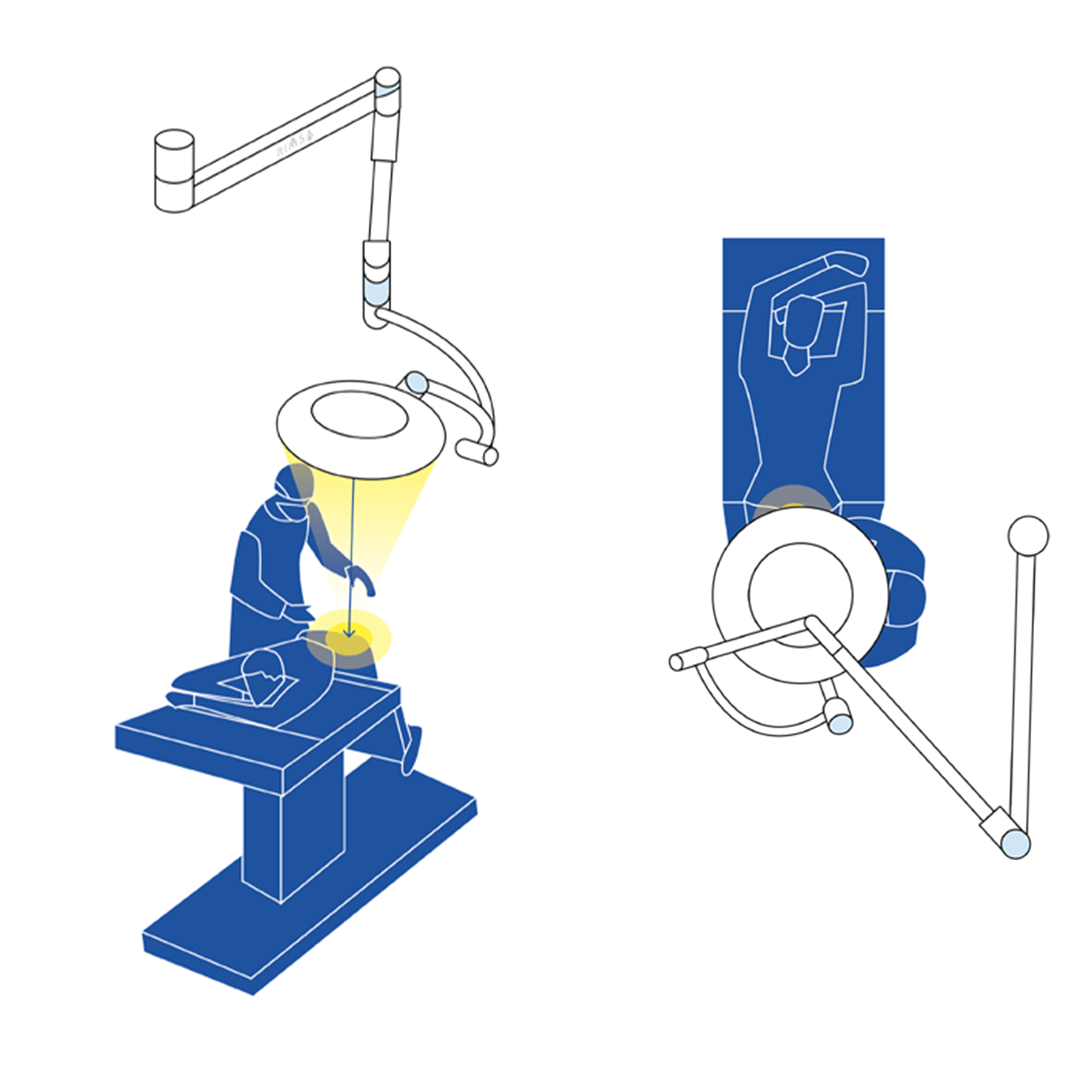
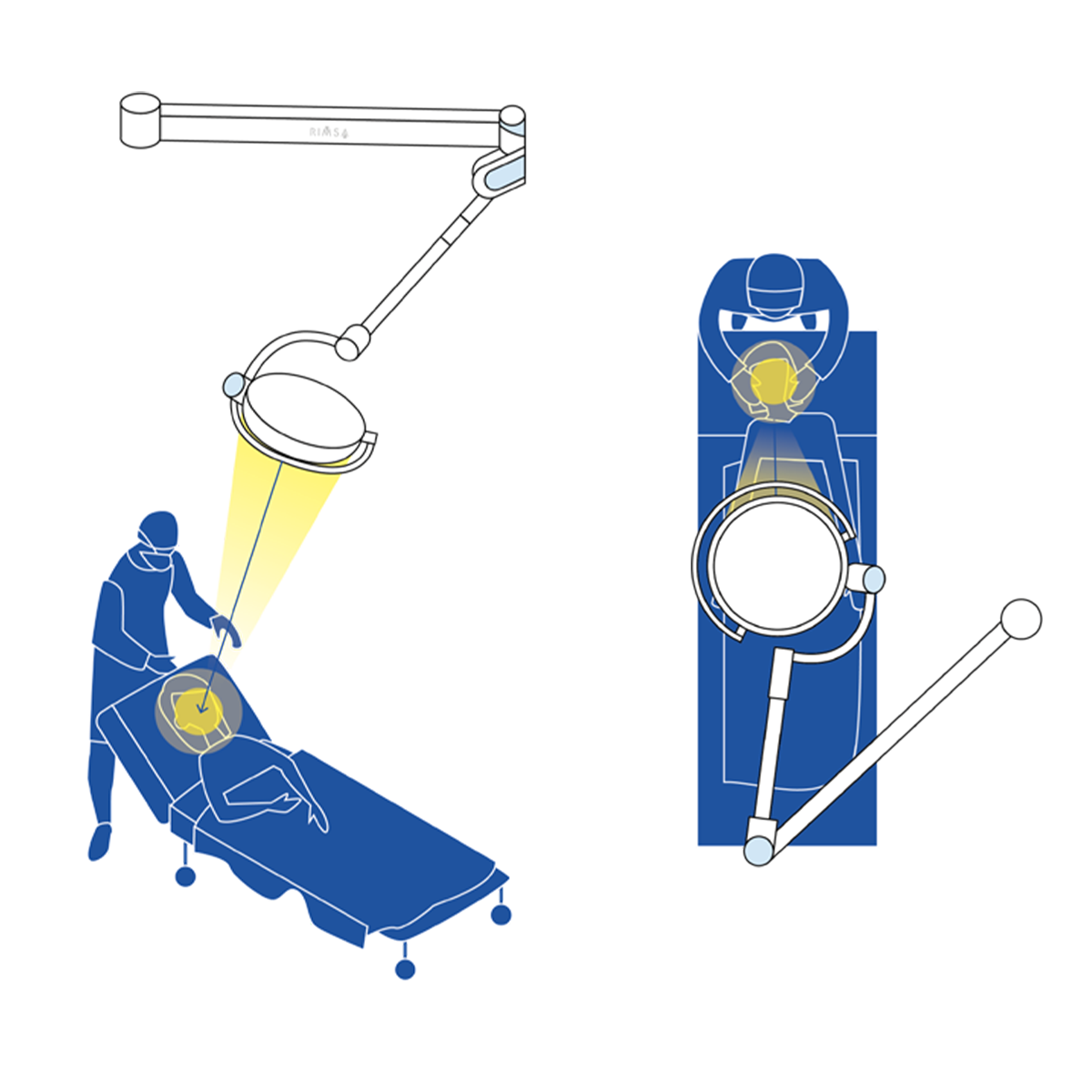
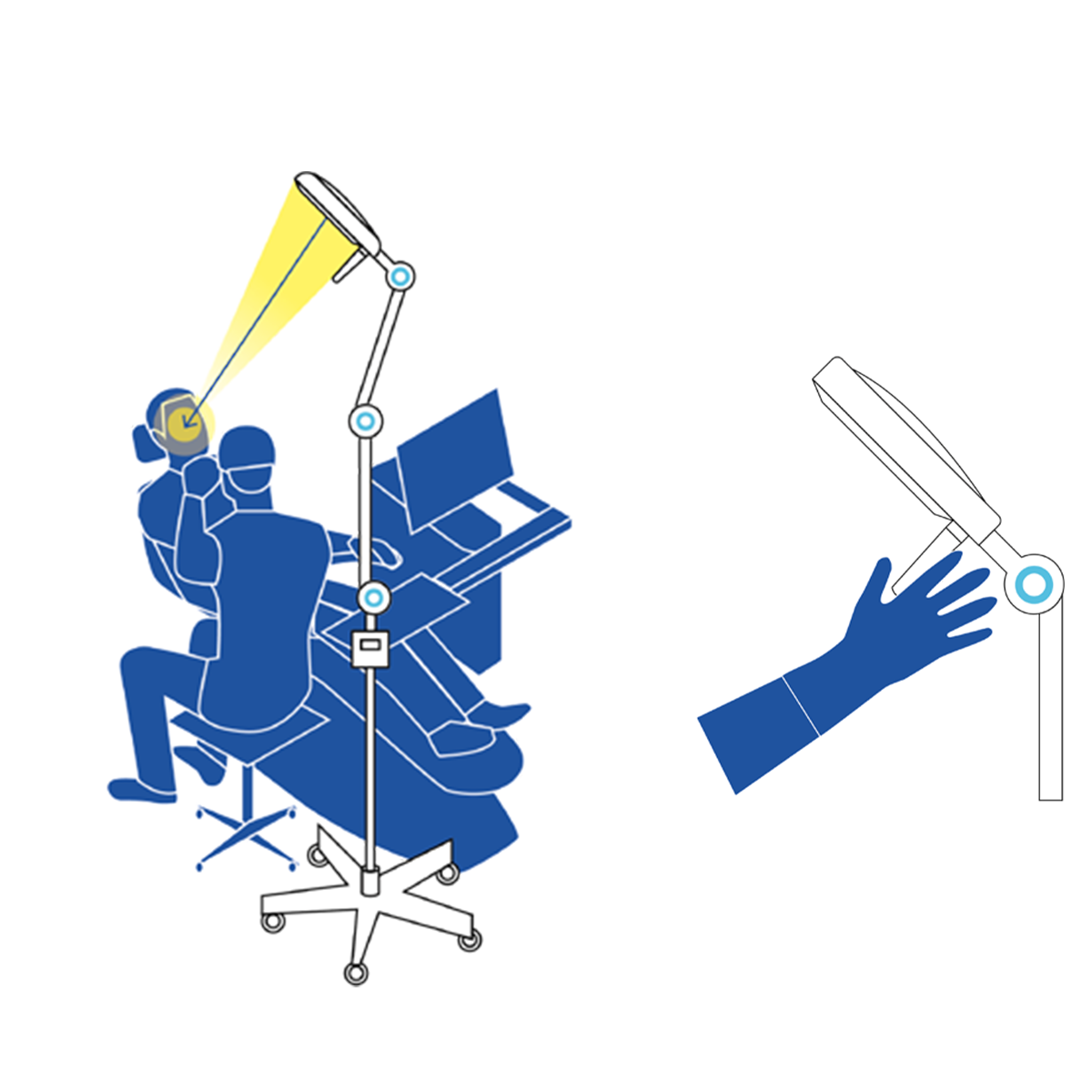
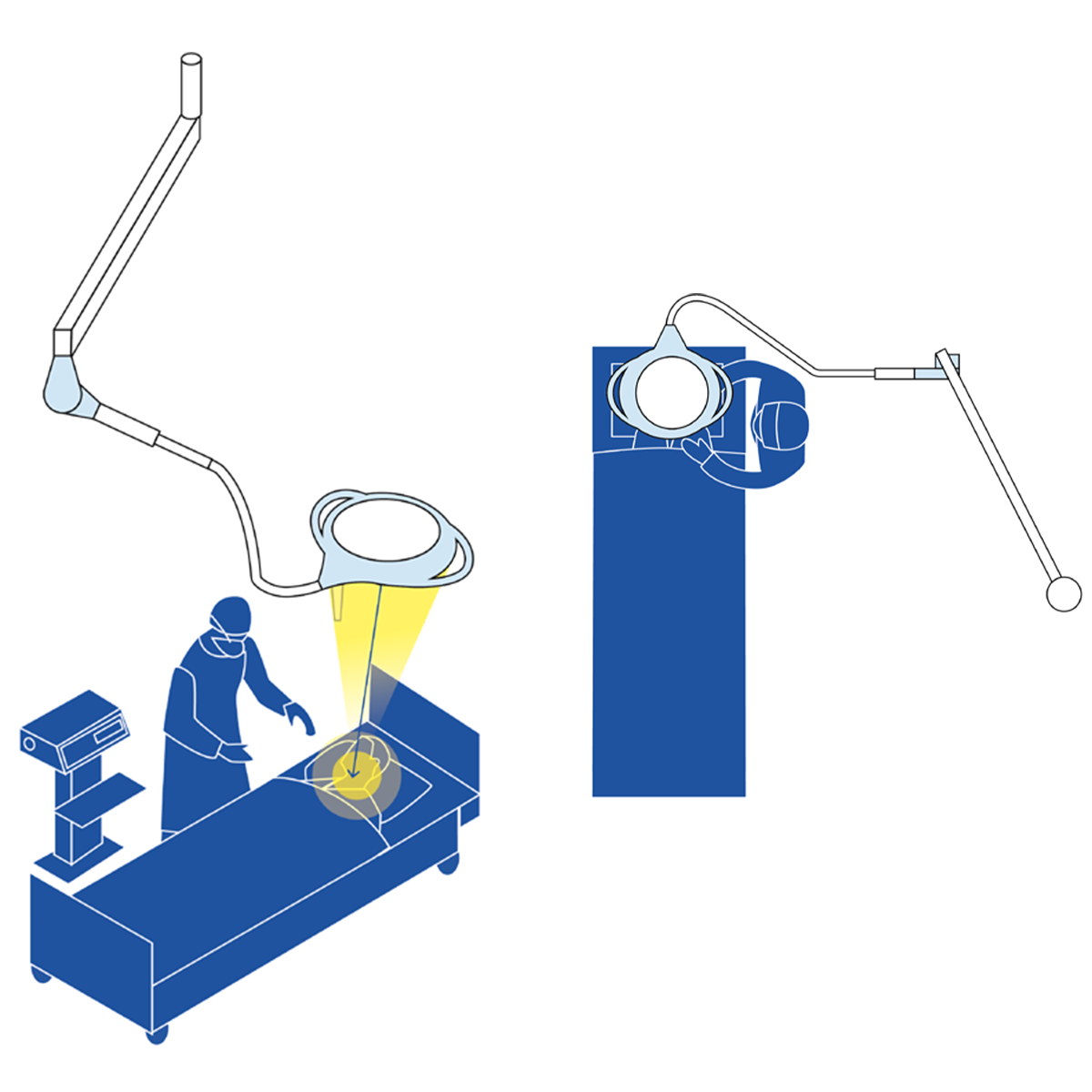
Whether in an operating theater or an intensive care unit, surgical lighting is crucial for creating a comfortable environment for both physician and patient. RIMSA lamps ensure homogeneous, consistent illumination of the work area, delivering a highly intense beam of light that highlights every detail:
– Surgeons are supported at every step of their work.
– Patients benefit from a welcoming, reassuring atmosphere where they feel at ease and secure before undergoing surgery.